Description of the pathology
Mechanism of injury and defense of the body
Traditional treatment
Kinesis treatment
Description of the pathology
THE ATTACHMENT SYNDROME
This syndrome has several synonyms such as: encroachment, conflict so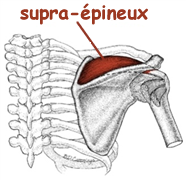 us-acromial, tendinitis of the rotator cuff, butting as well as impingement.
us-acromial, tendinitis of the rotator cuff, butting as well as impingement.
To fully understand the impingement syndrome, it must be remembered that the shoulder is a joint that has several structures contained in a limited space.
The shoulder is a very mobile joint whose bony structures fit together poorly since the humeral head is too large for the glenoid cavity of the scapula (scapula). This difference in size causes instability (the shoulder is therefore more prone to injuries such as dislocations). In order to counter this instability, the muscles of the shoulder play a major role and must work harmoniously and efficiently to solidify and stabilize the shoulder. To be most effective, the stabilizing muscles must not only be sufficiently strong and flexible, but they must also contract and relax at specific times in the movement.
Among these stabilizing muscles, the most important are grouped together under the name of “the rotator cuff”. As the name suggests, these muscles cap and wrap the shoulder and serve to stabilize the humeral head in the glenoid. These muscles initiate the movement by allowing the bones to be well centered and oriented in the direction of the desired movement.
The rotator cuff is made up of four muscles. The one that is most often injured is the supraspinatus (formerly called supraspinatus). teres minor). Although the long portion of the biceps is not officially part of the rotator cuff, it plays an important functional stabilizing role because its tendon is intracapsular (implanted deep into the joint).
The impingement syndrome is defined by the supraspinatus tendon rubbing on the coracoacromial ligament, thus creating irritation at the level of the tendon. The pain appears on the front side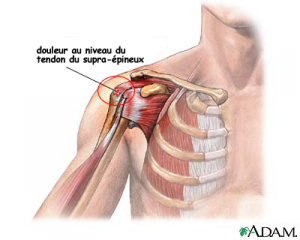 of the humerus.
of the humerus.
The movements of flexion (raising the arm forward), abduction (raising the arm to the side) and external rotation of the shoulder (turning the arm outward) become restricted and painful.
The following are examples of painful movements that can trigger impingement syndrome:
- A. Everyday movements:
1) Fasten the bra at the back (stretching pain)
2) Comb your hair
3) Screw in a screw at shoulder height or higher
4) Turn a doorknob
- B. Sports gestures:
1) Swimming: In the crawl, the action of bringing the arm back just before the hand enters the water and, sometimes, during the pull (movement of the arm in the water)
2) Canoe: Just before plunging the paddle into the water
3) Volleyball: Just before impact and during impact when spiked or served
4) Tennis: During service
As we mentioned above, the supraspinatus is part of the group of muscles called "the rotator cuff" and are intended to stabilize the humeral head in the glenoid (which is the shoulder joint).
The mechanism of injury is often associated with a repetitive motion such as in sports or occupations where the arm passes overhead (e.g. baseball, tennis (serve), volleyball (smash), swimming, water polo , painter, carpenter, bricklayer, lineman etc.).
The irritation often occurs on the supraspinatus tendon in the acromiohumeral outlet (the space between the humeral head, acromion, and coracoacromial ligament). Because of this irritation, our body is forced to "repair" the lesion created by the rubbing of the tendon. This repair (or inflammation) creates more fibrous and thicker tissue (scar) which decreases the space inside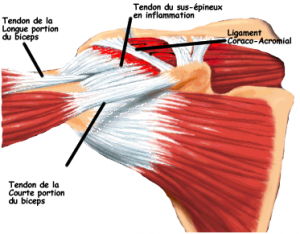 inside the acromial gorge. If this situation is not corrected quickly, the syndrome can progress and become chronic. This could create a small vicious circle; swimming motion, tendon irritation on the coraco-acromial ligament (due to tighter space), inflammation (repair of damaged tissue) which leads to scar tissue (thicker tissue) and the process repeats itself.
inside the acromial gorge. If this situation is not corrected quickly, the syndrome can progress and become chronic. This could create a small vicious circle; swimming motion, tendon irritation on the coraco-acromial ligament (due to tighter space), inflammation (repair of damaged tissue) which leads to scar tissue (thicker tissue) and the process repeats itself.
Pain causes our brain to want to protect the injured area by causing the rotator cuff to spasm to prevent movement of the shoulder (glenohumeral joint).
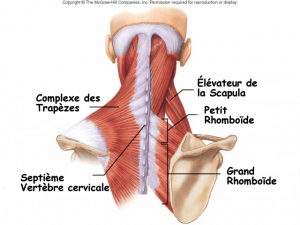
If we don't act quickly enough, the spasm can spread to the stabilizers of the scapula: the g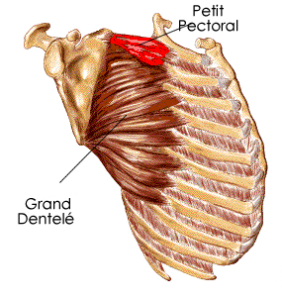 serratus rand, pectoralis minor (two muscles located at the front), levator scapulae, rhomboids and trapezius group (muscles located at the back).
serratus rand, pectoralis minor (two muscles located at the front), levator scapulae, rhomboids and trapezius group (muscles located at the back).
 The point of all of this is to make all the structures around the shoulder as still as possible (like a cast) to allow full healing.
The point of all of this is to make all the structures around the shoulder as still as possible (like a cast) to allow full healing.
To illustrate the appearance of an impingement syndrome, let us cite the example of an elite swimmer who trains for the crawl. During this type of swimming, the number of strokes performed per week is phenomenal. Movements above the head, repeated many times, (during the recovery phase and pulling the arm) can easily irritate the tendon of the supraspinatus by friction.
Imagine a swimming pool of Olympic size, therefore a pool of 50m deep. th length.
th length.
A top crawl swimmer will perform between 20 to 28 strokes per length. These swimmers will train for 5-8 km per workout and will do between 8 and 12 workouts per week in the pool, i.e. they will swim approximately 50 km per week.
Knowing that you have to cover 20 pool lengths in a 50m pool in order to cover 1km, running 50km is like doing 1000 lengths. 1000 lengths times 24 strokes per length represents no less than 24 strokes per week. (For the crawl and the backstroke, the use of the arms is alternated (unilateral) so we divide this number by 000: which amounts to performing 2 strokes per arm per week). This means that the supraspinatus tendon passes close to the coracoacromial ligament 12 times a week.
In addition to this movement repeated thousands of times in the water, we must not forget that technical errors and fatigue during training can cause an imperfect movement that will cause unnecessary stress on the structures. In addition, bad postures, lack of flexibility or muscle imbalance, anatomical peculiarities (more pronounced acromion and therefore less space for the tendon), muscle strengthening overload, previous injuries, inadequate sleeping position , etc… will also influence the shoulder of this swimmer. Taking into account the movements related to his sport and his daily life, we have to admit that several factors can irritate the tendon and thus cause pain, spasms and functional decrease in the swimmer.
Once the problem sets in...
The pain appeared. She is really unpleasant, intrusive. It prevents us from doing our favorite sport, from performing. It ruins our lives, even when we are not moving. It interferes with our sleep and ends up affecting our character…What to do?
Should we consult and if so, who to consult? Will the pain go away on its own? Should we take medicine or undergo medical tests? How many treatments will be needed to regain our well-being and function? Should we continue my sport?
The first thing you need to know is that each case is different. The human being may resemble each other from one individual to another, the fact remains that everyone has their own system of regulation and reactions. What works for one may be completely useless or even harmful for someone else. We must therefore learn to know ourselves and come to recognize what is good for us.
It is always difficult to know where to turn to manage our injury. There are so many therapies and styles of therapists it can be overwhelming. And, if I took a break, wouldn't the problem and all its annoyances magically disappear, as they appeared?
In the acute phase, the primary goal of the traditional approach is pain relief (by controlling inflammation). The prescription of an anticapitalist. »>anti-inflammatory will therefore be considered in almost all cases, for a period of approximately two weeks. Like any injury in the acute phase, the GREC rules will be advised to the patient: Ice / Rest / Elevation of the injured limb / Compression. In other words, we avoid painful movements, effort and we apply ice at least three times a day (waiting 2 hours between each application) for a maximum of 20 minutes and we must repeat this protocol for approximately two weeks. It is not uncommon for the patient to leave the doctor's office with a prescription for physiotherapy in their pocket; generally sessions twice a week for three to six weeks will be recommended.
The role of the Kinesis Center therapist during the first visit is to reduce pain to allow the nervous system to slow down its body's protective mechanisms. Before explaining this role to you in the face of pain and the protective mechanisms, we must understand the latter.
Our first goal will therefore be to reduce pain to allow the patient's nervous system to lower its guard quickly. In this way, the patient will avoid being caught in the infernal vicious circle of the body's protective mechanism.
The protective mechanism is normal and even desirable for a short period of time (acute phase), but after a few days it should disappear. If it is still present after a few weeks, the cycle of chronic pain manifests itself and the vicious circle becomes a painful reality affecting our quality of life.
Here is how the cycle can be experienced:
All the symptoms experienced during the cycle lead to a decrease in the quality of life.
To reduce inflammation and pain, we use a variety of therapies.
Thanks to the needlesacupuncture placed along the meridians, the acupuncturist obtains a response from the nervous system which allows the spasms to be released. Acupuncture also improves circulation and energy promoting recovery. An electric current can also be added to increase the effectiveness of the technique. Generally, the benefits of acupuncture are felt quickly from the first appointment.
La fasciatherapy specific allows amazing results. It allows us to create space in the soft tissues around the supraspinatus tendon allowing the evacuation of metabolic waste. Indeed, the inflammatory process and, consequently, that of healing degrade chemical agents and these debris end up accumulating in the affected region. Specific fasciatherapy is a gentle method that allows us to release and open the fascia. It's as if we stretched an envelope that was too tight, preventing us from breathing well and circulating the blood well. Another image that clearly explains the effect of fasciatherapy is a corset that is too tight and unfastened. Tissues become less tight, blood and lymphatic circulation improve. The region will be better nourished and better cleaned.
Le sports physiotherapist will carry out very specific work at the site of the injury, i.e. the supraspinatus, its synergists (infraspinatus, teres minor), its antagonist (subscapularis) as well as the stabilizers of the scapula (rhomboids, trapezium complex, serratus anterior and levator scapulae). Using local fasciatherapy and myofascial stretching techniques, the sports physio will manage to relax the muscles and their envelopes to create space and reduce protective spasms. Once the protective scheme has been eliminated and the pain gone, the sports physiotherapist will reprogram the parameters of the stabilizing muscles of the rotator cuff through specific proprioceptive exercises. On average, three to five appointments should be scheduled to properly manage this problem. The sports physio will call on these colleagues in acupuncture, osteopathy or shiatsu to supplement if necessary.
THEosteopathy, mainly because of its cranial therapy, helps reduce tension, pain and inflammation at a distance.
Once the inflammation and pain are controlled, our goal will be to relax the muscle associated with the tendon, i.e. the supraspinatus, with techniques of bringing together and light myofascial stretching (we are talking about here of myofascial therapy). We will continue our work towards a more global relaxation by aiming to relax the synergist muscles (the muscles that help the affected muscle to perform its movement: infraspinatus, teres minor and subscapularis).
The treatments will then be oriented so that the person regains their normal joint mobility at the level of the structures connected to the shoulder such as the cervical and dorsal column, the ribs, the sternum, the clavicles. To work at joint level, you can consult the masso-kinesitherapists or osteopaths.
To work more in depth, because the organs (because of their nerve, ligament and fascial links) can also influence the mobility of the shoulder, see an osteopath.
Once mobility and flexibility are back, the ball is in your court to sustain the return to sport and active living without pain. A program of proprioception, posture, breathing, stretching and strengthening exercises (if muscle imbalances have been found) will get you off to a good start. Sports massage therapists specializing in sports rehabilitation can teach you everything.
Information on the protection mechanism?

Leave a Reply
Want to join the discussion?Feel free to Contribute!